
📊 Tyler Olsen
This story first appeared in the October 2, 2024, edition of the Fraser Valley Current newsletter. Subscribe for free to get Fraser Valley news in your email every weekday morning.
The situation at BC’s most-overcrowded large hospital has grown considerably worse in the last five years.
Abbotsford Regional Hospital was already operating well over capacity in 2019, before the pandemic hit. Five years later, though, the facility’s decade-old congestion issues have hit yet another dismal peak, according to figures obtained by The Current.
Last year, the Fraser Valley’s largest hospital operated at 128% capacity over the entirety of the 2023/24 fiscal year. Essentially, for every four admitted patients for which the hospital had capacity, ARH’s staff also had to find space for—and time to treat—one additional person. That statistic is the worst of any major BC hospital in the last decade.
But it’s more than just a number; it reflects the very real state of ARH’s care wards. Last week, the challenges prompted a group of doctors to publicly decry the situation, noting that patient beds are sometimes placed in shower areas.
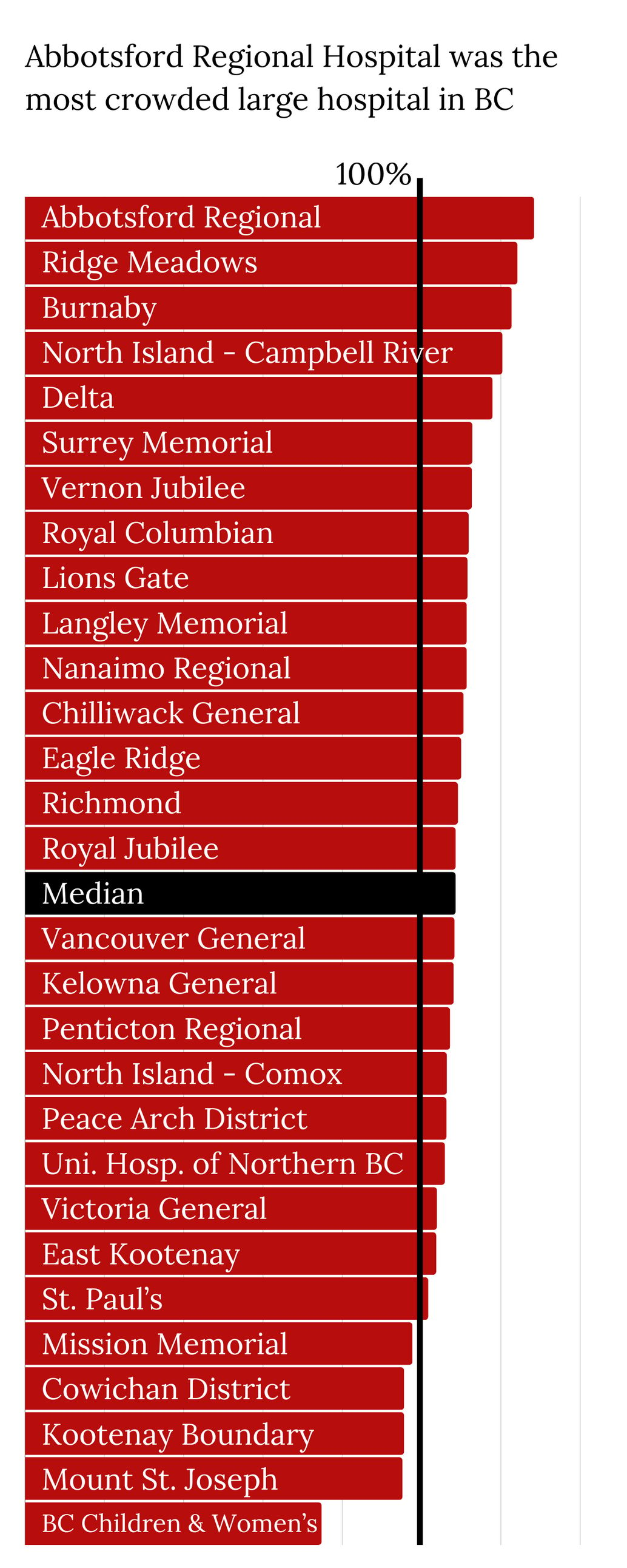
The situation at ARH is extreme, but hardly unique, according to the data obtained by The Current. Two dozen other health care facilities across BC also had occupancy rates above 110%. That group included hospitals in Langley and Chilliwack.
The congestion
You can find a table with five years of capacity figures for every hospital in BC at the bottom of this story.
With the brief exception of the first year of the pandemic—when the province rushed to empty health care facilities to make room for potential influxes of patients and reduce in-facility transmission—British Columbia’s hospitals have been operating over capacity for more than a decade.
In 2017, in the wake of two incidents in which patients died after being sent home from ARH’s emergency room, I requested and received a half-decade’s worth of data on hospital capacity. The data showed the entrenched depth of crowding challenges in BC’s hospitals: since at least 2012, the entire system had been operating over capacity, with more patients than it had the staff, space, and money to treat.
That initial investigation also turned up warnings from health officials that operating above 95% capacity increases risks to patients. Hospital capacity challenges manifest themselves differently depending on the patient. A funded hospital bed is not just a bed—it’s also the infrastructure and human resources that goes into creating a space for a patient. So when a hospital—or an entire hospital system—is over capacity, that leaves patients in places that are not designated for care. There, they are frequently treated by nurses and doctors who have more patients than would be considered ideal. Yesterday, the chief executive officer of a Vancouver Island health foundation said that some patients at Nanaimo’s hospital are treated in spaces that used to be closets. *
But seven years later, and despite a new government taking charge of BC’s health system, the congestion challenges have only grown worse. Today, BC’s hospitals are even more crowded.
The congestion issues have been particularly striking at the province’s largest Lower Mainland hospitals. In addition to Abbotsford’s hospital, Royal Columbian Hospital, Burnaby Hospital, Langley Memorial Hospital, and Vancouver General Hospital are all typically over capacity and more-crowded than before the pandemic.
Within that group, Abbotsford Regional Hospital stands out for both the severity of the congestion and its persistence. Five years ago, the hospitals in Chilliwack and Abbotsford were the most-crowded big facilities in the province with annual occupancy of around 115%. The situation at Chilliwack General Hospital has modestly improved, although the facility still operated at 110% capacity last year. But crowding has grown significantly worse at ARH. Last year’s occupancy rate of 128% means that on any single day, the hospital had nearly twice as many surplus patients as it did five years earlier. Fraser Health did add 25 beds to the hospital, but that won’t fix the situation; on average, Abbotsford Regional Hospital had around 60 more inpatients than it had beds in 2022/23.
A provincial spokesperson acknowledged in an email in July that occupancy rates across all BC’s health authorities have been above 100% for the last two years. The Current subsequently asked for regionwide capacity numbers, and was told they would be provided. The spokesperson subsequently stopped responding to emails. After contact with another spokesperson was made by phone last week, The Current was told no information could be provided because the provincial election campaign had begun.
Correction: This story originally incorrectly said a health authority CEO said some patients at Nanaimo’s hospital are treated in spaces that used to be closets. In fact, the statement was made by the CEO of the Nanaimo and District Hospital Foundation.
The causes
The problem isn’t actually the sheer volume of patients, but the severity and persistence of their ailments.
In 2022/23, the most recent year for which The Current has inpatient data, BC’s hospitals treated slightly fewer inpatients as they had before the pandemic.
But those inpatients stayed a half-day longer, on average, than patients five years ago. That resulted in an 8% increase in total inpatient days—and the total demand on BC’s hospital beds. That jump was felt across all five of British Columbia’s regional health authorities.
The province did respond. By last November, the province had boosted the number of funded beds across BC by nearly 8%. Health care spending also increased at a rapid pace, as the province poured money into fixing the crisis. (We will have a story on the dramatic increase in health care spending later this week.)
But it’s unclear whether the new beds, or the money that has thus far been spent, will actually reduce congestion, or if it can only mitigate the ongoing challenges.
In 2019/20, the median occupancy rate for BC’s 29 largest hospitals (those with at least 80 beds as of 2019) was 104.6%. That figure hit 108% in 2022/23 and ticked up slightly, to 108.6%, last year.
Story continues below

The increase in inpatient days and the resulting congestion is not simply the result of sicker or older patients—although that’s likely part of the problem. They also reflect a lack of health care support and facilities beyond hospitals. More than one in 10 inpatients BC don’t actually need to stay in hospital, even though they need continuing care. Instead, every day, thousands of patients lie in hospitals, waiting for a bed to open up in a different type of facility—frequently at a long-term care home. As those patients occupy acute care beds and wards, newly admitted patients can be forced to wait days in the emergency room or in inadequate and makeshift spaces where they are subject to cramped conditions and receive treatment from staff just trying to keep their heads above water.
British Columbia is building long-term care homes, but the need is massive. The province’s population of seniors over the age of 80 is expected to grow by 100,000 by 2030. In the 2030s, BC will have an additional 190,000 seniors.
The province and its health authorities are already working to build new long-term care homes in Langley, Abbotsford and Chilliwack with between 200 and 300 beds. But congestion figures show that ratio isn’t enough.In 2023, BC had roughly one provincially funded long-term care bed for every nine residents over 80. That ratio already appears to be insufficient, but just to keep up with its aging population (at its current insufficient level, BC will need to add around 10,000 beds over the next decade. That works out to opening nine such facilities every year for the next 16 years.
As the 2024 election campaign continues, the major parties have all declared their intention to “fix health care,” by recruiting more nurses and doctors and building more facilities. History, though, suggests that making such promises is infinitely harder than delivering actual improvements.
This story first appeared in the October 2, 2024, edition of the Fraser Valley Current newsletter. Subscribe for free to get Fraser Valley news in your email every weekday morning.

